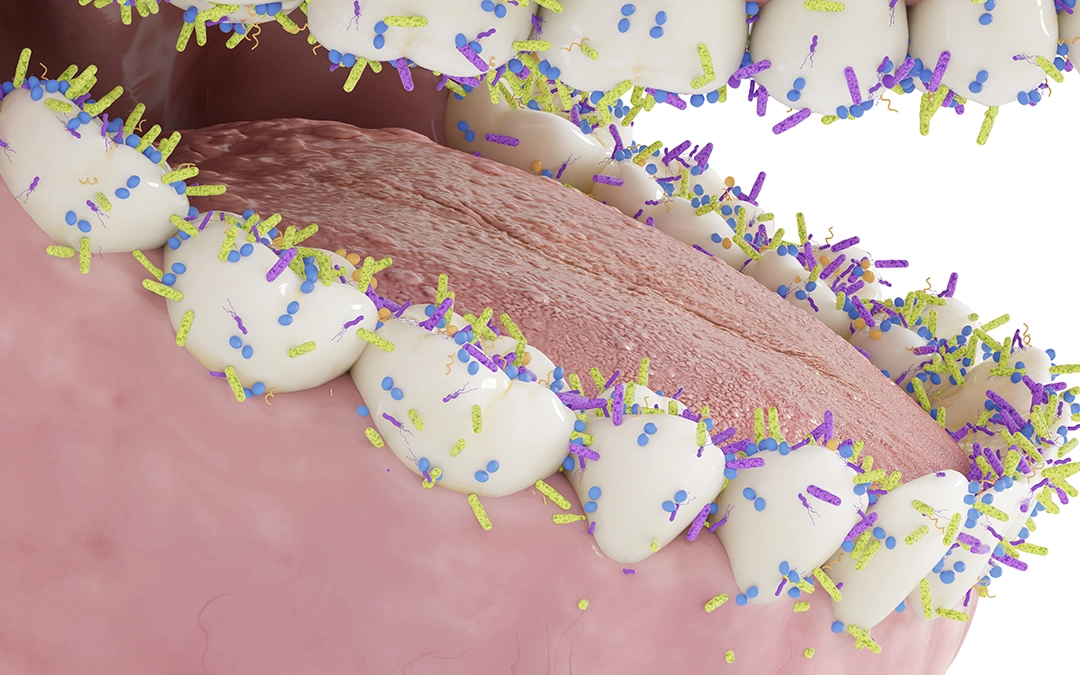
Did you know that our mouth hosts over 700 different species of bacteria? This microscopic ecosystem exists in delicate balance—while many of these microorganisms are beneficial guardians of oral health, others can trigger tooth decay, gum disease, and even affect overall well-being.
Our mouth serves as more than just a gateway for nutrition and communication; it’s a complex biological community where microbial populations constantly interact. The equilibrium of this oral microbiome significantly impacts our dental health and, surprisingly, our systemic health as well.
Understanding the behaviour of these bacteria and how your daily habits influence their population dynamics empowers you to make informed choices that protect your smile and long-term health.
What’s really living in our mouth?
Our mouths harbour a thriving microbial universe, where billions of bacteria continuously grow, reproduce, and interact. This intricate oral microbiome acts as a vital ecosystem, influencing oral health and overall general wellbeing.
Two main types of oral bacteria
Beneficial (commensal) bacteria
These microorganisms help protect against harmful invaders, aid in digestion, and maintain a balanced pH in the mouth.
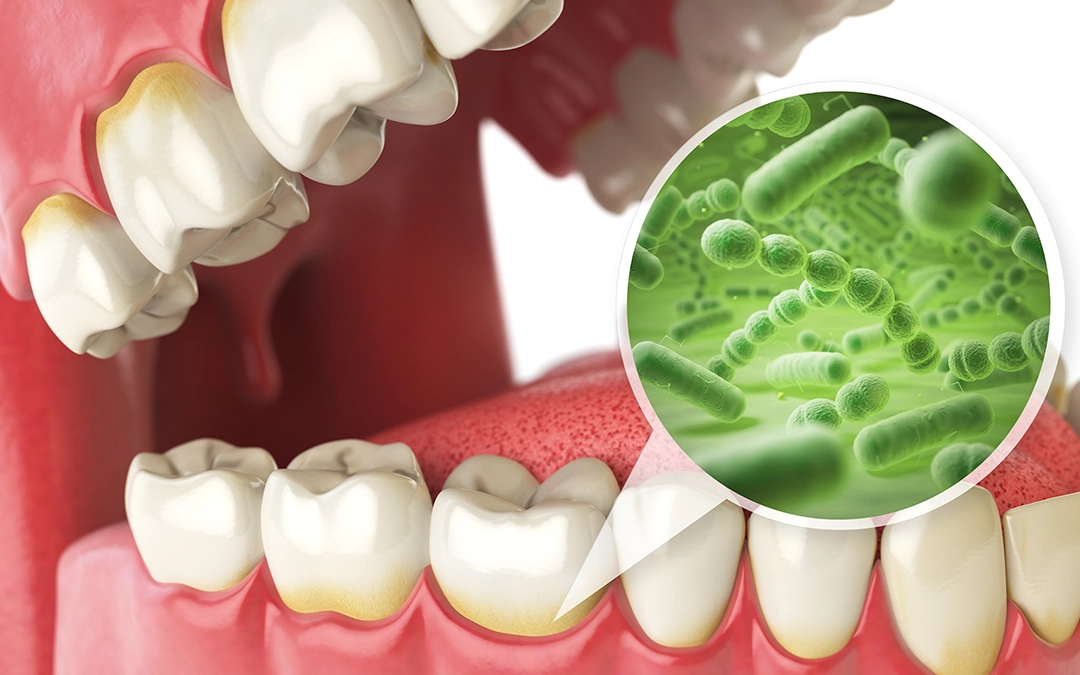
Harmful (pathogenic) bacteria
These bacteria produce acids and toxins that erode enamel, inflame gums, and contribute to infections.
The delicate bacterial balance
The health of our oral cavity depends on maintaining homeostasis (the body’s way of staying balanced and stable) between these bacterial populations. When diet, hygiene habits, or other factors disrupt this balance, harmful bacteria gain a competitive advantage, increasing the risk of oral diseases.
Emerging research highlights a strong connection between oral microbiota and gut health. These ecosystems communicate through complex pathways, meaning imbalances in one may reflect or even influence conditions in the other. This microbial interplay underscores the importance of oral health in maintaining overall systemic wellbeing.
Guardians vs. disruptors of oral health
Your mouth’s microbiome functions as a dynamic ecosystem where beneficial and harmful bacteria exist in a perpetual state of competition. Much like your gut microbiome, this delicate oral balance determines whether your mouth remains healthy or develops disease.
Beneficial bacteria:
These microscopic oral allies serve essential protective functions:
- Create a biological shield by occupying surface space that would otherwise host pathogens
- Maintain neutral pH levels by neutralising acids and preventing demineralisation
- Release natural antimicrobial compounds that specifically target harmful species
- Participate in the initial phases of digestion through enzymatic breakdown of complex carbohydrates
- Communicate with your immune system to regulate inflammatory responses
Harmful bacteria:
When conditions favour their growth, these opportunistic bacterial invaders can:
- Streptococcus mutans metabolises dietary sugars into acids that dissolve mineral content in tooth enamel, creating cavities
- Lactobacillus species thrive in acidic environments, further contributing to enamel erosion and cavity progression
- Porphyromonas gingivalis release enzymes that break down gum tissue and trigger chronic inflammation
- Treponema denticola penetrate deeper periodontal tissues, contributing to bone loss and advanced gum disease
- Anaerobic bacteria convert proteins into sulfur compounds, resulting in persistent halitosis that brushing alone cannot eliminate
The difference between ‘good’ and ‘bad’ bacteria isn’t always clear-cut. Some types play helpful roles when there are enough of them, but become harmful when they dominate your mouth. This complex relationship shows us why keeping a diverse balance of bacteria in your mouth, rather than just getting rid of them, is the real key to lasting oral health.
Signs your oral bacteria might be harming you
Is your mouth’s bacterial balance off? While your mouth naturally hosts a diverse bacterial community, an imbalance favouring harmful bacteria can cause several concerning indicators. Recognising these early warning signs allows for timely intervention before minor issues progress to serious oral health complications.
- Persistent bad breath
- Bleeding or swelling gums
- Frequent cavities or tooth sensitivity
- White or yellow coating on the tongue
- A persistent bad taste in the mouth
- Reduced salivary flow (dry mouth)
- Frequent mouth sores

Contributing factors to bacterial imbalance
Your daily choices significantly influence which bacterial populations thrive in your oral environment. Frequent sugar consumption fuels acid-producing bacteria, leading to enamel erosion and cavities. Poor oral hygiene allows plaque to mature into hardened tartar, creating a breeding ground for harmful microbes. Smoking depletes oxygen levels in the mouth, promoting the growth of disease-causing bacteria, while chronic stress weakens the immune system, reducing its ability to keep bacterial populations in check.
Left unaddressed, these factors contribute to gum disease and other oral health complications. This is why maintaining a balanced oral microbiome is essential for long-term health.
How oral bacteria impact overall health
The bacteria residing in your mouth don’t respect boundaries—they can migrate throughout your body, potentially triggering or worsening serious health conditions, like heart disease or diabetes. This oral-systemic connection (the connection between oral and overall health) represents one of healthcare’s most significant changes in understanding, transforming our understanding of how seemingly isolated infections influence distant organ systems. This is why proactive oral health care is more important than ever.
Conditions linked to harmful oral bacteria:
Cardiovascular disease
Oral pathogens can enter the bloodstream through inflamed gum tissue, adhering to arterial walls and triggering inflammation that accelerates atherosclerosis. This bacterial presence is linked to an increased risk of coronary artery disease, heart attacks, and strokes. Research suggests individuals with periodontal disease face up to three times higher risk of cardiovascular events.
Diabetes management
The relationship between diabetes and oral health is bidirectional—periodontal inflammation exacerbates insulin resistance, destabilising blood sugar levels, while elevated glucose fuels bacterial overgrowth, worsening gum disease. Studies show that diabetic patients who manage their periodontal health experience measurable improvements in HbA1c levels, highlighting the importance of oral care in metabolic control.

Respiratory vulnerability
Aspiration of oral bacteria can introduce harmful microorganisms into the lungs, leading to secondary infections. In high-risk groups—especially the elderly and immunocompromised—this bacterial transmission significantly increases the likelihood of aspiration pneumonia and worsens conditions like COPD (chronic obstructive pulmonary disease).
Pregnancy outcomes
Maternal periodontal disease elevates systemic inflammation, potentially triggering premature labour and restricting foetal growth. Studies indicate that pregnant women with active gum disease face higher risks of preterm birth and low-birthweight infants, emphasising the importance of periodontal health during pregnancy.
Neurodegenerative connections
Recent studies have identified Porphyromonas gingivalis—a key periodontal pathogen—in the brain tissue of Alzheimer’s patients. Research suggests that these bacteria may contribute to beta-amyloid plaque formation, potentially playing a role in the inflammatory processes linked to cognitive decline.
Oncological associations
Chronic oral inflammation may create an environment conducive to malignant transformation. Studies have found significant associations between periodontal disease and increased risks of certain cancers, including colorectal, pancreatic, and oesophageal malignancies. While the exact mechanisms are still being explored, ongoing research continues to uncover the potential links between oral and systemic oncology.

How to maintain a healthy oral microbiome
Keeping your oral bacteria in check requires a combination of good hygiene, a balanced diet, and regular dental care.
1. Prioritise daily oral hygiene
✔ Brush twice daily with fluoride toothpaste to remove plaque buildup.
✔ Floss daily to clean areas where a toothbrush can’t reach.
✔ Use a tongue scraper to reduce bacterial accumulation.
✔ Use an antimicrobial mouth rinse (if prescribed by your dentist).
✔ Replace your toothbrush every three months to prevent bacterial buildup.
2. Adopt a diet that supports a healthy oral microbiome
✔ Incorporate probiotic-rich foods (yoghurt, kefir, fermented vegetables) to encourage good bacteria.
✔ Eat fibre-rich foods to stimulate saliva production and naturally cleanse the mouth.
✔ Consider oral probiotics to help restore beneficial bacterial balance.
✗ Reduce sugar intake, as it fuels cavity-causing bacteria.
✗ Avoid frequent snacking, which provides a continuous food source for harmful bacteria.
3. Stay hydrated
✔ Drinking plenty of water supports saliva production, which neutralises acids and washes away bacteria.
4. Quit smoking and reduce alcohol consumption
✗ Smoking disrupts the oral microbiome and increases the risk of gum disease.
✗ Excessive alcohol consumption dries out the mouth, reducing saliva’s protective effects.
5. Visit your dentist regularly
✔ Routine checkups & professional cleanings help prevent bacterial overgrowth.
✔ Early detection of oral health problems can prevent them from becoming severe or costly.

Optimise your oral health for total wellbeing
Your mouth harbours a sophisticated microbial universe where billions of organisms form an ecosystem that profoundly influences oral health and general wellbeing. A balanced oral microbiome helps defend against harmful bacteria, reducing the risk of serious conditions like cardiovascular disease, diabetes complications, and Alzheimer’s disease.
By prioritising excellent oral hygiene and making mindful lifestyle choices, you’re not just maintaining a bright, healthy smile—you’re actively protecting your long-term health. Take control of your wellbeing today. Visit your dentist and invest in a healthier future.
What small steps can you take right now to support a thriving oral microbiome? Start today—your future self will thank you!
References
Benn, A. M. L., Heng, N. C. K., Broadbent, J. M., & Thomson, W. M. (2018). Studying the human oral microbiome: Challenges and the evolution of solutions. Australian Dental Journal, 63(1), 14–24. https://doi.org/10.1111/adj.12565
Bostanghadiri, N., Kouhzad, M., Taki, E., Elahi, Z., Khoshbayan, A., Navidifar, T., & Darban-Sarokhalil, D. (2024). Oral microbiota and metabolites: Key players in oral health and disorder, and microbiota-based therapies. Frontiers in Microbiology, 15, 1431785. https://doi.org/10.3389/fmicb.2024.1431785
Deo, P. N., & Deshmukh, R. (2019). Oral microbiome: Unveiling the fundamentals. Journal of Oral and Maxillofacial Pathology, 23(1), 122–128. https://doi.org/10.4103/jomfp.JOMFP_304_18
Hernández-Cabanyero, C., & Vonaesch, P. (2024). Ectopic colonization by oral bacteria as an emerging theme in health and disease. FEMS Microbiology Reviews, 48(2), fuae012. https://doi.org/10.1093/femsre/fuae012
Li, X., Liu, Y., Yang, X., Li, C., & Song, Z. (2022). The oral microbiota: Community composition, influencing factors, pathogenesis, and interventions. Frontiers in Microbiology, 13, 895537. https://doi.org/10.3389/fmicb.2022.895537
Rajasekaran, J. J., Krishnamurthy, H. K., Bosco, J., Jayaraman, V., Krishna, K., Wang, T., & Bei, K. (2024). Oral microbiome: A review of its impact on oral and systemic health. Microorganisms, 12(9), 1797. https://doi.org/10.3390/microorganisms12091797



