How to treat snoring and sleep apnoea in comfort
Groggy, irritable, and unable to focus—that’s no way to wake up! When you suffer from snoring and sleep apnoea, you can wake up exhausted even after a full night’s sleep. That can take a serious toll on your overall health and quality of life, but rest assured that change is in the air. Over the years, treatment strategies have evolved, providing patients with more effective and comfortable solutions. While continuous positive airway pressure (CPAP) therapy has long been the standard treatment, modern advancements, such as oral appliances, now offer compelling alternatives.
Snoring and sleep apnoea
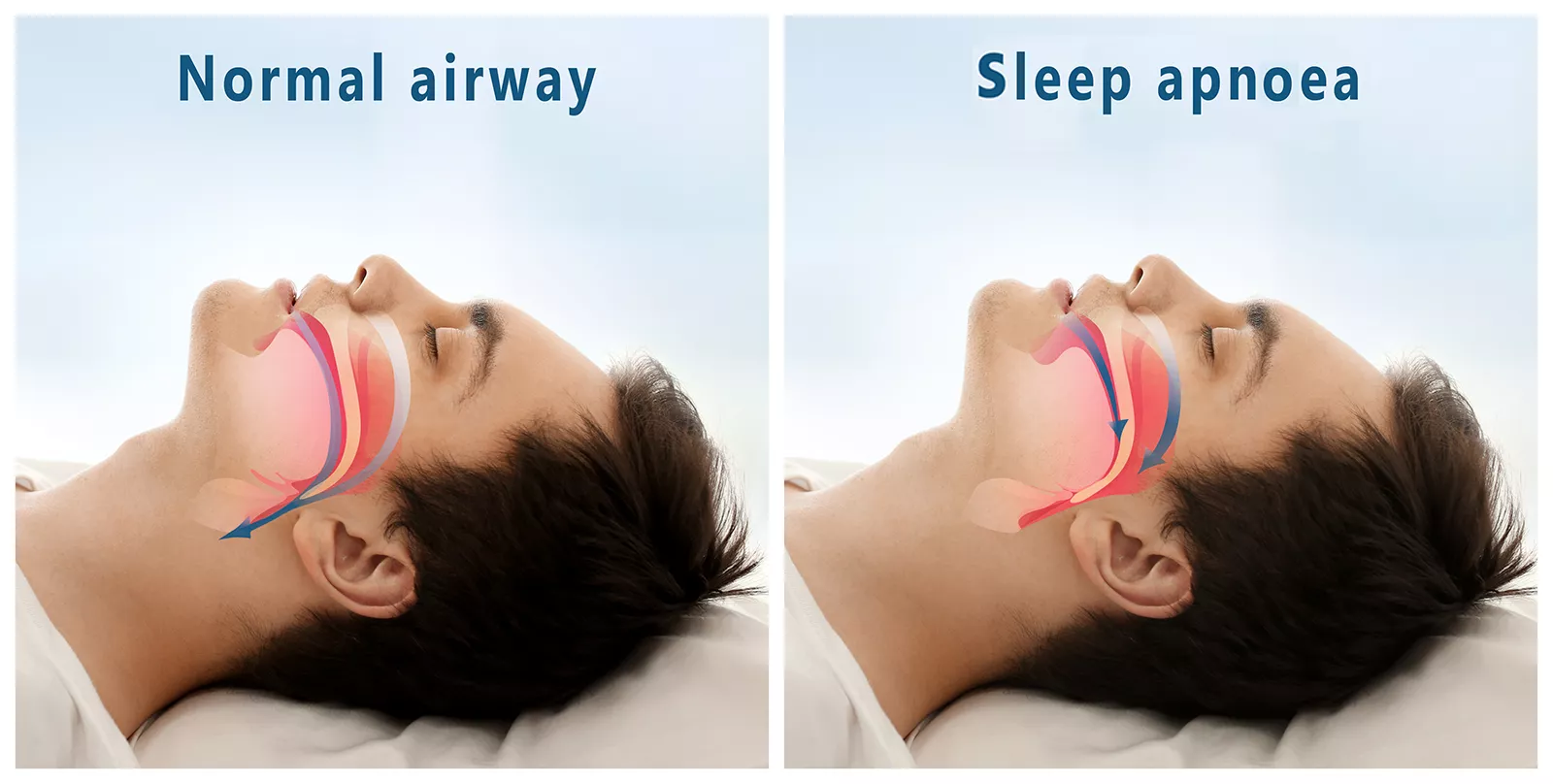
Snoring happens when airflow is partially blocked during sleep, causing vibrations in the soft tissues of the throat, leading to the familiar, often disruptive noise. While occasional snoring may be harmless, persistent snoring can be a warning sign of obstructive sleep apnoea (OSA)—a serious condition where the airway repeatedly collapses, reducing oxygen intake and disrupting sleep cycles. Left untreated, OSA can lead to significant health risks and long-term complications.
Untreated sleep apnoea has been linked to serious health risks, including:
- High blood pressure
- Heart disease
- Stroke
- Type 2 diabetes
- Daytime fatigue and cognitive impairment
Traditional treatment: CPAP therapy
For decades, CPAP therapy has been the go-to solution for moderate to severe sleep apnoea. By delivering a steady stream of pressurised air through a mask, CPAP prevents airway collapse, allowing for continuous, uninterrupted breathing throughout the night. While highly effective, its practicality and comfort remain points of concern for many patients.
Benefits of CPAP therapy:
- Highly effective in maintaining an open airway
- Reduces apneic episodes and improves blood oxygen levels
- Enhances sleep quality and overall health
Challenges of CPAP therapy:
- Many patients find the mask uncomfortable and difficult to tolerate
- Common issues include noise, dryness, and restricted movement during sleep
- Compliance rates can be low, particularly for mild to moderate OSA sufferers

Surprisingly comfortable oral appliance therapy
In recent years, oral appliance therapy (OAT) has emerged as a game-changer for individuals with mild to moderate obstructive sleep apnea (OSA) or those struggling with CPAP therapy. These custom-fitted devices, crafted by dentists trained in sleep medicine, gently reposition the lower jaw and tongue to keep the airway open during sleep. Unlike CPAP machines, oral appliances are compact, silent, and easy to wear, making them a preferred choice for many patients seeking a more comfortable and practical solution.
There are several types of oral appliances designed to manage sleep apneoa, with Mandibular Advancement Splints (MAS’) being the most preferred.
Mandibular Advancement Splints (MAS’)
These devices are designed to reposition the lower jaw forward, which helps prevent the airway from collapsing during sleep. By advancing the mandible (lower jaw), MAS’ ensure that the tongue and soft tissues do not obstruct the airway, effectively reducing snoring and improving airflow for those with moderate OSA. MAS’ are often made from flexible, durable materials and are custom-fitted to each patient’s unique dental structure.
Alongside CPAP and oral appliances, snoring and sleep apnoea treatment often includes:
Positional therapy: Encourages sleeping in positions that reduce airway obstruction.
Surgical interventions: Procedures such as Uvulopalatopharyngoplasty (UPPP) and Inspire therapy (hypoglossal nerve stimulation) offer solutions for severe cases.
Lifestyle modifications: Weight loss, avoiding alcohol before bed, and nasal breathing exercises can help reduce symptoms and improve sleep quality.
Tongue-Stabilising Devices (TSDs): work by gently holding the tongue in a forward position, preventing it from collapsing into the airway during sleep.

How dentists help people sleep better
Dentists specialising in sleep medicine play a crucial role in the management of snoring and sleep apnoea. Through detailed evaluations of oral and airway structures, they design and fit custom oral appliances tailored to each patient’s needs. Beyond just providing the device, they offer ongoing adjustments and monitoring to ensure long-term effectiveness and comfort. Working in close collaboration with sleep physicians, dentists help develop comprehensive, patient-centred treatment plans that improve sleep quality and overall health.
What to expect at a dental visit for sleep apnoea:
1. Comprehensive evaluation, including a review of symptoms and medical history
2. Referral for a sleep study
3. Digital impressions or scans to create a custom oral appliance
4. Fitting and adjustments for maximum comfort and effectiveness
5. Follow-up to monitor progress and make necessary refinements

Enjoy restful sleep night after night
Newer treatment strategies for snoring and sleep apnoea empower patients with more choices than ever before. While CPAP remains a reliable solution for severe cases, oral appliances provide a comfortable, effective alternative for those with mild to moderate OSA. With expertise in sleep medicine, dentists play a vital role in helping patients regain restful sleep, improve their health, and enhance their overall quality of life.
Don’t let snoring or sleep apnoea mess with your well-being. Schedule a consultation with your dentist today to find your ideal personalised treatment options so you can wake up feeling fresh and energetic every day.
Almeida, F. R., & Bansback, N. (2013). Long-term effectiveness of oral appliance versus CPAP therapy and the emerging importance of understanding patient preferences. Sleep, 36(9), 1271–1272. https://doi.org/10.5665/sleep.2938
Benjamin K. Tong, Carolin Tran, Andrea Ricciardiello, Michelle Donegan, Alan K. I. Chiang, Irene Szollosi, Jason Amatoury, Jayne C. Carberry, & Danny J. Eckert. (2020). CPAP combined with oral appliance therapy reduces CPAP requirements and pharyngeal pressure swings in obstructive sleep apnea. Journal of Applied Physiology, 129(5), 1085-1091.
Doff, M. H., Hoekema, A., Wijkstra, P. J., van der Hoeven, J. H., Huddleston Slater, J. J., de Bont, L. G., & Stegenga, B. (2013). Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: A 2-year follow-up. Sleep, 36(9), 1289–1296. https://doi.org/10.5665/sleep.2948
National Heart, Lung, and Blood Institute. (2025). Sleep apnea. https://www.nhlbi.nih.gov/health/sleep-apnea
NHS. (2022). Sleep apnoea. https://www.nhs.uk/conditions/sleep-apnoea/



